What Causes Heart Attacks?
Jul 17, 2023
What Causes Heart Attacks?
Written by Sandeep Singh, MD FACC in Coronary Heart Disease

A heart attack basically means the heart muscle was deprived of oxygen carrying hemoglobin resulting in damaged tissue. This is usually caused by an interruption of blood flow, most often caused by a blockage in the artery (or arteries) supplying the heart muscle. Blockages are more often caused by plaque buildup (cholesterol, fat) though can be caused by other things.
What is Atherosclerosis?
This is a process (also called arteriosclerosis) that occurs over many years, where cholesterol and fatty deposits localize to the wall of an artery, progressively damaging it, causing the formation of a plaque that can rupture or occlude a blood vessel.
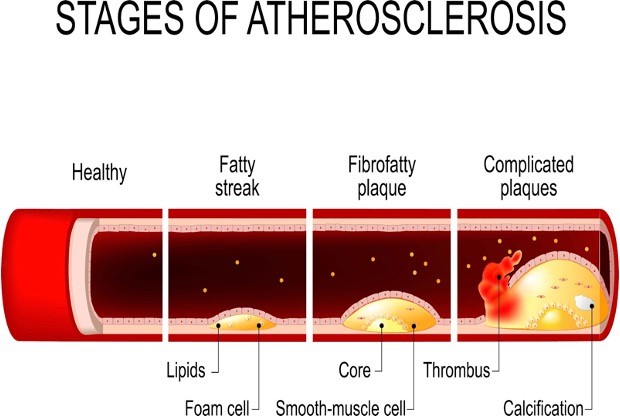
This causes the blood vessels to become thickened and stiff, further limiting blood flow to an organ or tissue. Normal healthy arteries are elastic and are able to dilate when extra blood flow is necessary. Diseased arteries cannot adequately respond to an increased demand in blood flow.
Over time, these arteries that have become thicker, stiffer and laden with cholesterol plaque, become calcified. This is where the term “Hardening of the Arteries” comes from. Calcium is “hard” as in bone. When it deposits on the arteries, they become “hard”.
There is a test available that can actually look for early evidence of this calcification process referred to as a Coronary Calcium Score.
Symptoms of a Heart Attack
Symptoms can vary widely. From none or minimal symptoms to what is referred to as sudden cardiac death. In between these two extremes are what we find most commonly. Most people have some form of chest discomfort. This can translate into shooting pains, chest burning or an ache, or even shortness of breath. The classic set of symptoms of a heart attack are:
- Chest heaviness or pressure, that often radiates into the left arm, neck or jaw
- Nausea
- Sweaty
- Shortness of breath
How Do You Diagnose a Heart Attack?
The initial test to diagnose a heart attack is usually an electrocardiogram (ECG or EKG). It’s a cheap, quick way of detecting certain electrical signals that suggest there is an acute heart attack (also called an acute myocardial infarction) in progress.

Certain electrical patterns can suggest which artery might have the blockage, and thus directing a particular course of action such as a cardiac catheterization where a stent might be placed to open the artery and restore blood flow.
How Do You Treat a Heart Attack?
The initial therapy for most people having a heart attack often starts with an aspirin or other anti-platelet agent, a blood thinner, and sometimes a cholesterol agent and a beta blocker.
The type of heart attack will usually determine which treatment gets offered first. The two large categories of heart attack are:
- Completely obstructed artery, usually resulting in a “STEMI” or ST Elevation Myocardial Infarction. This type of heart attack is usually best treated by performing a cardiac catheterization so that a percutaneous coronary intervention (or PCI) can be performed. This is a procedure that is performed in the cardiac catheterization lab (aka cath lab) that involves the placement of a coronary stent.
- Partially obstructed artery, usually resulting in a “NSTEMI” or Non-ST Elevation Myocardial Infarction. This type of heart attack is usually treated initially with medication, but may also involve proceeding to the cardiac cath lab to see if a coronary stent is needed. If multiple arteries are blocked or if the left main coronary artery is severely diseased, then coronary artery bypass grafting or surgery (CABG) may also be required.
Once the acute phase of the heart attack is over and the patient has been stabilized, then the medication regimen usually involves the following agents:
|
Medications often used during and after a heart attack |
|
|
|
|
|
Can I Get Another Heart Attack?
Unfortunately, once you’ve had a heart attack, you are at higher risk for a second. But that doesn’t mean you can’t take matters into your own hands and reduce that risk!
By changing your lifestyle and eating habits, you can have a profound effect on your risk of future disease or more events. Most people realize they could live healthier and as a result, trade out their old habits for new, better ones.
In fact, most people end up losing weight in the months following their heart attack. Fear is a great motivator.
Unfortunately, the vast majority of people end up resorting to old habits and gain that initial weight back within the first year.
About one in five people end up back in the hospital with their second heart attack within the first 5 years of their first one. This amounts to about 350,000 people each year with a recurrent heart attack. That’s alot of people!
Can You Prevent a Heart Attack?
Maybe.
Heart attacks are non-discriminating, equal opportunity players. Marathon runners can get them, older people and younger people. Men, women, people of all races are eligible.
I like to compare a higher risk of a heart attack to a higher risk of getting struck by lightning. If there’s a thunderstorm happening outside, and you decide to walk into it with a tall, metal rod, then you INCREASE your chances of of getting struck by lightning.
– Dr. Singh
Likewise, if you don’t exercise, eat poorly, smoke cigarettes, have poorly controlled diabetes or high blood pressure, then you are in essence, INCREASING your risk, walking around with a tall metal rod waiting to get struck, but by a heart attack.
|
Steps to take to lessen your chances of having a heart attack |
|
|
|
|
|
|
|
|
I wish I could say that by doing all the right things you can eliminate your risk of a heart attack, but that’s unfortunately not the case. As stated above, even marathon runners can be at risk for having a heart attack. Likewise, just because you don’t smoke, doesn’t mean that you cannot get lung cancer.
If you have a strong genetic history of heart disease, you can lessen or delay your risk by taking better care of yourself, but you cannot eliminate it. And once you’re above a certain age, family or genetic predispositions matter much less.
The clear and convincing evidence is that the earlier in life you take good care of yourself, the less your risk of having a cardiac event will be later in life.


