What is Atrial Fibrillation?
Jul 17, 2023
What is Atrial Fibrillation?
Written by Sandeep Singh, MD FACC in Arrythmia (Heart rhythm disturbances)

Atrial fibrillation (often referred to as Afib) is an electrical rhythm disorder of the heart that can increase the risk of a stroke in those with the appropriate risk factors.
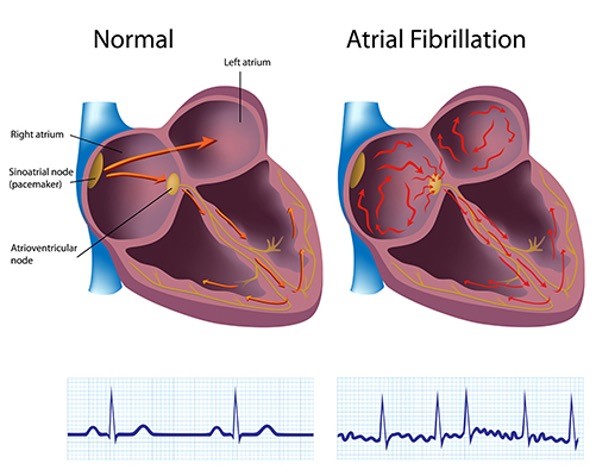
The upper chambers of the heart referred to as the atria (there are two), normally contract in a synchronized fashion to push blood to the lower chambers of the heart, known as the ventricles. In the rhythm atrial fibrillation, the upper chambers are no longer contracting in a synchronized fashion and as a result, blood no longer gets pushed to the lower chambers and thus can clot. The upper chambers (atria) are beating erratically while in atrial fibrillation.
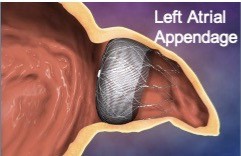
Clots that form in the atria (most commonly in the left atrium in a section called the left atrial appendage) can then travel to the brain causing a stroke, as well as to the kidneys, intestines, and even the heart itself.
Symptoms of Atrial Fibrillation
A significant number of patients who experience atrial fibrillation, unfortunately, will either have no symptoms or present with a stroke as their first symptom.
Others may feel a rapid, forceful, or irregular heartbeat sensation often referred to as palpitations. Some may report shortness of breath, chest discomfort, or even loss of consciousness.
Any sign or symptom of a stroke should always make us consider atrial fibrillation as a potential cause, and hence try and search for it. Atrial fibrillation can be fleeting. It can be there one moment and disappear shortly thereafter.
Please be aware that MOST people with palpitations do NOT have atrial fibrillation.
Palpitations more often represent a less concerning change in heart rhythm (such as premature atrial or ventricular contractions).
How Do You Diagnose Atrial Fibrillation?
Any form of heart rhythm monitoring could potentially identify atrial fibrillation.
The most common way is with a simple electrocardiogram or ECG (a.k.a. EKG).
If you are in a hospital setting often one will be on a heart monitor which can pick up this rhythm. We also have many forms of heart monitors one can wear (24 hour, 48 hour, 7 day, 14 day, or 30 day long monitors).
There is even an implantable heart monitor that is the size of a tiny chip that gets placed under your skin that can monitor your heart rhythm for up to three years! And it can be monitored remotely via an internet connected box that interfaces with the implanted monitor to keep close tabs on your heart!
Nowadays, we have several wearable devices that also have the ability to identify a change in heart rhythm.
The Apple Watch, along with the Samsung watch (Galaxy Watch3 and Galaxy Watch Active2), in addition to other wearables will become more sophisticated and be able to alert us in real-time as to any change in heart rhythm. Presently, although they are able to discern between normal sinus rhythm and atrial fibrillation, they still cannot do so with a high degree of accuracy.
There is also a smartphone accessory known as Kardia Mobile that can identify and monitor you for any changes in heart rhythm. Although not a wearable, it provides for another form of heart rhythm assessment and can be particularly useful for those who have symptoms of rapid or irregular heartbeats that occur too infrequently to be detected on a standard rhythm event monitor mentioned above.

Kardia Mobile
An experienced Cardiologist can also identify atrial fibrillation by listening to your heart, although this would always be corroborated with an electrocardiogram.
How Do You Treat Atrial Fibrillation?
There are several ways to treat atrial fibrillation that depend on the age, kidney and liver function, heart condition as well as whether they have symptoms of atrial fibrillation versus whether it was found incidentally by rhythm monitoring.
The first step in choosing what therapy someone needs is to assess their risk of having a stroke. We use a formula referred to as the CHA2DS2VASc Score. This is a way of determining who needs a blood thinner such as Eliquis, Xarelto, or Coumadin (aka Warfarin). If the score is >= 2 then the recommendation is to start one of these blood thinners. Although aspirin is commonly thought of as a blood thinner, it is not adequate nor optimal to use aspirin as a therapy in lessening the risk of stroke from atrial fibrillation. Aspirin, however, can help reduce risk in coronary heart disease, especially in those who already suffer from this diagnosis.
|
CHA2DS2VASc Score |
|
|
Congestive Heart Failure |
+1 |
|
Hypertension |
+1 |
|
Age >65 yo |
+1 |
|
Diabetes |
+1 |
|
Stroke (or TIA) |
+2 |
|
Vascular Disease |
+1 |
|
Age >75 yo |
+2 |
|
Sex Category (if Female) |
+1 |
The other medication approach to atrial fibrillation is using anti-arrhythmic drugs, usually in addition to anticoagulant medications, or using medications that will simply control heart rate to ensure that the heart rate remains controlled. If your heart rate remains too high for too long, this can result in weakening of your heart leading to congestive heart failure.
For many who experience atrial fibrillation for the first time, a quick and relatively safe way of restoring normal sinus rhythm is often employed. Direct current cardioversion (DC Cardioversion) is a method of applying a direct shock to the heart while the patient is under conscious sedation (under light anesthesia similar to that given during a colonoscopy). Recovery is quick and the patient then returns home shortly afterward.
Lastly, there are invasive therapies that can help lessen the burden of atrial fibrillation or even eradicate it. The radiofrequency ablation procedure involves inserting a catheter up into the heart where radiofrequency energy is applied to the areas where the Afib originates from. Often, more than one radiofrequency ablation procedure is necessary to fully ablate or eradicate the atrial fibrillation.
For those patients who cannot tolerate anticoagulant medications (blood thinners) due to prior bleeding issues, there is a procedure referred to as the Watchman procedure, which is a way to lessen the stroke complication aspect of atrial fibrillation. It is done in a similar fashion where a catheter is inserted into the heart, upon which is mounted a device, is inserted into the left atrial appendage, thus lessening the ability of a clot to form, thus lessening the risk of stroke.
How common is atrial fibrillation?
Atrial fibrillation is amongst the most common arrhythmias to occur, especially in older women. Approximately 10% of all individuals older than age 65 years of age will develop atrial fibrillation. This rhythm disorder, due to its association with stroke, is amongst the most impactful and burdensome heart conditions.
As technology advances, we will hopefully have even better tools to diagnose and treat this order. The consumer directed wearable devices are the most significant advance in detection, though much is still yet to be done.


